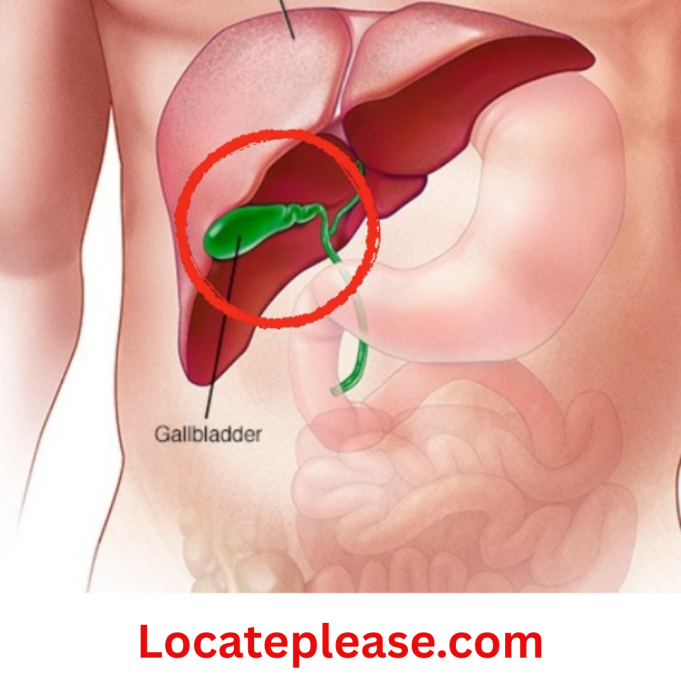
When we eat a rich, satisfying meal, our gallbladder does its quiet work—releasing bile to help digest fats and gently guarding our gut with its natural antibacterial power. It’s a small organ with a profound role: not just breaking down food, but protecting the delicate balance within us.
When gallbladder trouble arises—stones, inflammation, pain—it can feel like a trusted friend has turned against us. Many wonder: Should it stay or go? And if it must go, what then?
Let’s walk through this with honesty and grace—not to frighten, but to empower.
When Is Removal Truly Needed?
Not every gallstone requires surgery. Like a quiet neighbor who only occasionally stirs trouble, some stones live peacefully inside us.
Your doctor may recommend waiting if:
✓ Stones are small and cause no pain
✓ You have no fever, nausea, or digestive distress
✓ Ultrasounds show no signs of blockage or infection
Surgery may be wise when:
✓ Pain becomes frequent or severe (especially after fatty meals)
✓ Inflammation (cholecystitis) or infection (cholangitis) develops
✓ Stones block bile ducts, risking pancreatitis
✓ Your quality of life is deeply affected
This isn’t a failure of prevention—it’s wisdom in action.
Sometimes the kindest choice is to let go.
How Your Body Adapts After Surgery
Removing the gallbladder isn’t like losing a limb. It’s like rerouting a river—life finds a new flow. Most people heal well, but your body may need gentle guidance as it adjusts. Here’s what can happen—and how to work with your body, not against it.
1. Digesting Fats Requires Patience
Without its storage pouch, bile now drips steadily into your intestine instead of flowing in waves. This means:
→ Fats may feel heavier after meals
→ Greasy foods might cause bloating or discomfort
→ Your body learns to adapt—but slowly
Gentle support:
- Start with small portions of healthy fats (avocado, olive oil, nuts)
- Avoid fried foods for the first few months
- Consider an ox bile supplement if your doctor approves (helps replace lost storage)
2. Bile’s New Rhythm Changes Digestion
That steady drip of bile can sometimes:
→ Cause mild bloating or gas after meals
→ Make digestion feel less efficient
→ Alter how vitamins A, D, E, and K are absorbed
Gentle support:
- Eat smaller, more frequent meals (3 squares + 2 snacks)
- Cook vegetables until tender (raw salads may feel harsh at first)
- Ask your doctor about a multivitamin with fat-soluble vitamins
3. Gut Bacteria May Need Rebalancing
Bile isn’t just for digestion—it’s a gentle guardian of your gut’s delicate ecosystem. Without its rhythmic release:
→ Beneficial bacteria may struggle to thrive
→ Intestinal inflammation can sometimes increase
→ Sensitivity to certain foods may rise
Gentle support:
- Add fermented foods slowly (kefir, sauerkraut, kimchi)
- Consider a probiotic after consulting your doctor
- Prioritize fiber-rich foods (oats, sweet potatoes, berries) to feed good bacteria
4. Bile Reflux: A Quiet Discomfort
Sometimes, bile flows upward into the stomach, causing:
→ A bitter taste in the mouth
→ Heartburn that isn’t relieved by typical antacids
→ Nausea after eating
Gentle support:
- Avoid lying down for 3 hours after meals
- Skip tight clothing around the waist
- Sip ginger tea or chew fennel seeds after eating
- Ask your doctor about bile-binding medications if needed
5. Dietary Adjustments
Food isn’t the enemy—it’s your partner in healing. Many find their symptoms ease dramatically with mindful eating:
→ Embrace: Steamed vegetables, lean proteins, whole grains, cooked fruits
→ Limit gently: Fried foods, creamy sauces, excessive eggs, heavy dairy
→ Honor rhythms: Eat slowly, chew thoroughly, stop when 80% full
“After my surgery, I thought I’d never enjoy food again,” shared one woman. “But with small changes—broiled salmon instead of fried, roasted carrots instead of creamed—I found my way back to joy at the table.”
✨ 6. Sleep Disruptions
The shift in digestion can ripple into rest. Some people notice:
→ Waking between 1–3 a.m. (when the liver processes bile)
→ Restlessness or vivid dreams as the body adjusts
→ Anxiety around meal times affecting nighttime calm
Gentle support:
- Sip warm chamomile or lemon balm tea before bed
- Place a warm (not hot) rice sock on your abdomen to ease tension
- Keep dinner light and 3+ hours before sleep
- Practice 5 minutes of deep breathing in bed (inhale 4 counts, exhale 6)
Remember: This is often temporary. With consistent rhythms, sleep usually deepens within weeks.
✨ Three Conditions to Understand—Without Fear
After gallbladder removal, your body adapts—but wisdom lies in gentle vigilance. These conditions are not inevitable, but awareness helps us partner with our doctors for prevention.
1. Reflux Gastritis
Without concentrated bile releases, digestion slows. Fatty or hard-to-digest foods may linger, causing bile to flow backward into the stomach. This can irritate the lining, leading to:
→ Burning sensation after meals
→ Bitter taste in the throat
→ Nausea
Your gentle defense:
- Eat smaller portions of easily digested foods (see diet section below)
- Sleep with your head slightly elevated
- Discuss bile acid binders with your doctor if symptoms persist
2. Colon Health Considerations
Research suggests a small increased relative risk of colon issues after gallbladder removal. Why? When bile flows steadily (not in pulses), certain bile acids may interact differently with the colon.
Important nuance:
→ Absolute risk remains low for most people
→ This is not a reason to avoid necessary surgery
→ Prevention is powerful: high-fiber diets, regular screenings, and movement protect colon health far more than an intact gallbladder ever could
Your gentle defense:
- Prioritize 30g+ fiber daily (berries, flaxseed, cooked greens)
- Schedule colonoscopies as recommended by your doctor
- Move daily—even a 15-minute walk supports gut motility
3. Bile Duct Stones
Rarely, without the gallbladder’s storage role, the bile duct may dilate slightly, allowing stones to form. Modern surgical techniques minimize this risk, but awareness matters.
Signs to share with your doctor:
→ Sudden, severe upper-right abdominal pain after fatty meals
→ Pale stools or dark urine
→ Unexplained fever
Your gentle defense:
- Stay hydrated (water helps keep bile flowing)
- Follow your surgeon’s post-op care guidance
- Report any new, persistent pain promptly
💛 A quiet truth: Most people never develop these conditions. With mindful eating and regular check-ups, life after surgery is full and vibrant. Knowledge isn’t fear—it’s the quiet hand that guides you home.
✨ Nourishing Your Body Back to Balance
Food is your first medicine after surgery. These aren’t restrictions—they’re love letters to your healing body.
1. Easily Digestible Foods (Weeks 1–4)
Your gut needs rest to rebuild. Start gentle:
→ Days 1–2: Clear broths, applesauce, gelatin
→ Days 3–7: Scrambled eggs, oatmeal, steamed carrots, banana
→ Weeks 2–4: Baked chicken, rice porridge, mashed sweet potatoes
✅ Joye’s wisdom: “Think of your stomach like a tender seedling—nourish it with soft, warm foods until its roots grow strong.”
2. High-Quality Protein (Weeks 2–8)
Protein rebuilds tissue—but choose wisely:
→ Best: Poached fish, soft tofu, cottage cheese, egg whites
→ Later (Week 4+): Lean turkey, skinless chicken, lentil soup
→ Avoid: Tough meats, sausage, or fried proteins (hard to digest)
✅ Tip: Add a splash of lemon to fish—it aids digestion and brightens flavor.
3. Whole Grains & Gentle Fats (Ongoing)
Healing thrives on rhythm and variety:
→ Grains: Oat bran, quinoa flakes, millet (cooked until creamy)
→ Seeds/Nuts: Flaxseed meal (stirred into oatmeal), toasted sunflower seeds (start with 1 tsp)
→ Fats: Avocado slices, olive oil drizzled on cooked veggies
⚠️ Peanuts: While nourishing, introduce slowly—they can trigger reflux in sensitive people.
🌾 The art of eating now:
“Fill half your plate with cooked vegetables,
one-quarter with protein,
one-quarter with grains.
Eat until you’re 80% full—
leaving room for joy, not discomfort.”
✨ Your Recovery Rhythm: Discharge & Beyond
Modern laparoscopic surgery means gentle healing:
→ Most leave the hospital in 1–3 days
→ Discharge happens when you can:
✓ Tolerate clear liquids without nausea
✓ Walk steadily without dizziness
✓ Manage pain with oral medication
The first month at home:
- Weeks 1–2: Rest deeply. Walk 5 minutes every 2 hours. No lifting >5 lbs.
- Weeks 3–4: Gradually add cooked vegetables and soft proteins. Gentle stretching.
- Month 2: Resume light chores. Start short walks outdoors.
- Month 3: Most return to pre-surgery diets—if symptoms allow.
Guardians of your peace:
→ Avoid smoking (slows healing) and alcohol (irritates bile ducts)
→ Skip late nights—sleep is when your body repairs
→ Bundle up against drafts—your immune system is tender
→ Move gently: sway to music, stretch like a cat
“Three months after my surgery, I sat on my porch at dawn with a bowl of warm oatmeal and blueberries. My granddaughter said, ‘Mammaw, why are you smiling?’ I touched my healing scar and said, ‘Because my body remembered how to rest.’”
A Closing Thought
Life after gallbladder removal isn’t about loss.
It’s about rediscovery—learning your body’s new language, listening to its whispers before they become shouts.
This isn’t a broken body.
It’s a body that chose healing.
A body that deserves patience.
A body that still holds the capacity for joy, for fullness, for living well.
So honor its rhythms.
Adjust your plate with love.
And trust this truth:
The same wisdom that carried you through surgery
is already guiding your healing—
one gentle meal, one quiet breath,
one sunrise at a time.
—
With deep respect for your journey. 🌿
Note: This is general wellness information, not medical advice. Always consult your healthcare provider about your personal health journey.